The Hepatitis A virus may hijack an infected cell’s shipping machinery to fashion a cloak-like envelope. The finding shatters decades old dogma about viruses and may explain how HAV evades our immune system’s first responders
The Hepatitis A virus may hijack an infected cell’s shipping machinery to create a cloak-like envelope. Fashioned from the infected cell’s membrane, a team of researchers from the United States and South Korea found it may help the virus evade our immune system’s first responders.
“It’s really hard to find another example of a virus that does what HAV’s doing,” Dr. Stanley Lemon, study co-author and Professor of Medicine with the University of North Carolina at Chapel Hill, told SciFare.com. “We think this is really promoting the ability of the virus to spread in the host from liver cell-to-liver cell.”
Because HAV’s not known to have an envelope-like feature – a classic way of generally categorizing viruses – researchers have been accidentally tossing most of them out, for as long as they’ve been studying it.
The researchers said it might also explain why the virus separates from the rest of the infected sample in two different populations – one that represents the cloaked virus and one that doesn’t.
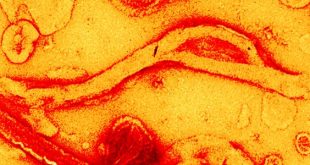
“We ended up looking at supernatant fluids that seemed to have some stimulatory activity by electron microscopy and we started seeing these particles wrapped in membranes,” Dr. Lemon said.
When they compared an alternative method to try and catch the elusive pouches, researchers found they could recover nearly 100 times more HAV than when they used traditional methods. In 12 experiments that followed, the team found that in roughly four out of every five HAVs in total, were cloaked and dodging them.
To researchers, they looked like exosomes – tiny packets that deliver proteins and RNAs after they bud-off from the cell membrane – and carried as many as four individual viruses per pouch.
“That led us to then look at the ESCRT system,” Dr. Lemon said. “[It’s] known to be involved in the production of classically enveloped viruses like influenza and HIV, as well as exosomes.”
One ESCRT protein that’s hijacked by enveloped viruses, known as VPS4B, provides the energy for the last kick out of the cell once other ESCRT proteins finish assembling the exosome. One such assembly protein, known as ALIX, helps in the manufacturing exosomes and other researchers have found that it’s necessary for other, enveloped viruses to bud-off from the infected cell.
When the researchers dialed down the amount of each protein to levels low enough to just prevent the cells from dying – known technically as a gene knockdown – they found both cloaked and uncloaked forms of HAV were prevented from exiting the infected cell.
On the protein coat that separates the envelope and protects HAV’s genetic material – known technically as its capsid – researchers even found two portions of the capsid protein VP2 that are similar to regions that HIV uses to interact with ALIX too.
“We found these two motifs that resemble those known to be present in other viruses that use ESCRT proteins,” Dr. Lemon said. “We suspect that those motifs in VP2 are part of the mechanism by which the virus begins to interact with the host elements involved in endosomal sorting.”
When they manipulated the two regions of VP2, so that it couldn’t interact with ALIX, the researchers found HAV lost its ability to fashion its cloak – it also impeded the assembly of its capsid.
The presence of a cloak-like cover may even explain some of the quirky features that have made the hepatitis A vaccine so effective.
“You can immunize an individual two weeks after exposure to hepatitis A and still have a high probability of preventing them from developing hepatitis,” Dr. Lemon said. “You’re not going to prevent the infection, but you do prevent the disease.”
It also challenges researchers to figure out where the battle between the vaccine and virus is taking place.
“It really raises significant questions about how this vaccine works,” Dr. Lemon said. “We believe that there’s neutralization occurring after the uptake of the enveloped particle into the cell.”
“That could be of significance in the future for the development of other virus vaccines,” he added.
Michael Houghton is a virologist at the University of Alberta and wasn’t part of the study. In an email to SciFare.com, he called the new research revolutionary because it shows the virus can exist in both forms.
“The virology field has always been broadly divided into enveloped and non-enveloped viruses and this paper blows up that dogma, which has existed for many decades,” Michael Houghton, who’s also a Canada Excellence Research Chair in Virology, said.
“This is a seminal piece of work and another clear demonstration of how long-held dogma can be overturned by both careful experimentation and alert, interpretation of data,” he added.
The new research was published in the journal, Nature.
 Science Fare Media Science News – Upgraded
Science Fare Media Science News – Upgraded